Introduction
The microbiome, or the microorganisms that impact the human body from within or on, can impact the health of a person in a multitude of ways. The introduction of AI and the growing utilization of next-generation sequencing (NGS) continue to unlock patterns between microbiota and disease states, including central nervous system (CNS) conditions.
Neurological conditions and diseases impact millions of individuals in the form of strokes, Alzheimer’s Disease, Parkinson’s Disease, epilepsy, and mood disorders, among others. While the exact degree to which the microbiome inhibits or primes the body for neurological conditions is yet to be understood, research indicates that this is a relationship worth investigating.
The Microbiome and the Brain
Several distinct microbial communities exist in symbiosis with the human body, including the gut. The gut microbiome plays a role in our neurological health via the gut-brain axis, a bidirectional pathway between the brain and the gut microbiome. Gut microbiota produce key metabolites and neurotransmitters, such as serotonin, while the brain modulates the microbiome through neural, endocrine, and immune mechanisms.
Interestingly, recent data challenges the notion of a sterile brain. While it is still up for debate whether these findings, which have identified microbial sequences in human brain samples, are artifactual; if true, they open up questions about the role microbiota play in neurological functioning.1 Even more groundbreakingly, some studies have found that certain neurological conditions / diseases may be associated with higher levels of certain bacteria in the brain (e.g., elevated Chlamydia pneumoniae and Alzheimer’s).2
Notable Commercial Activity
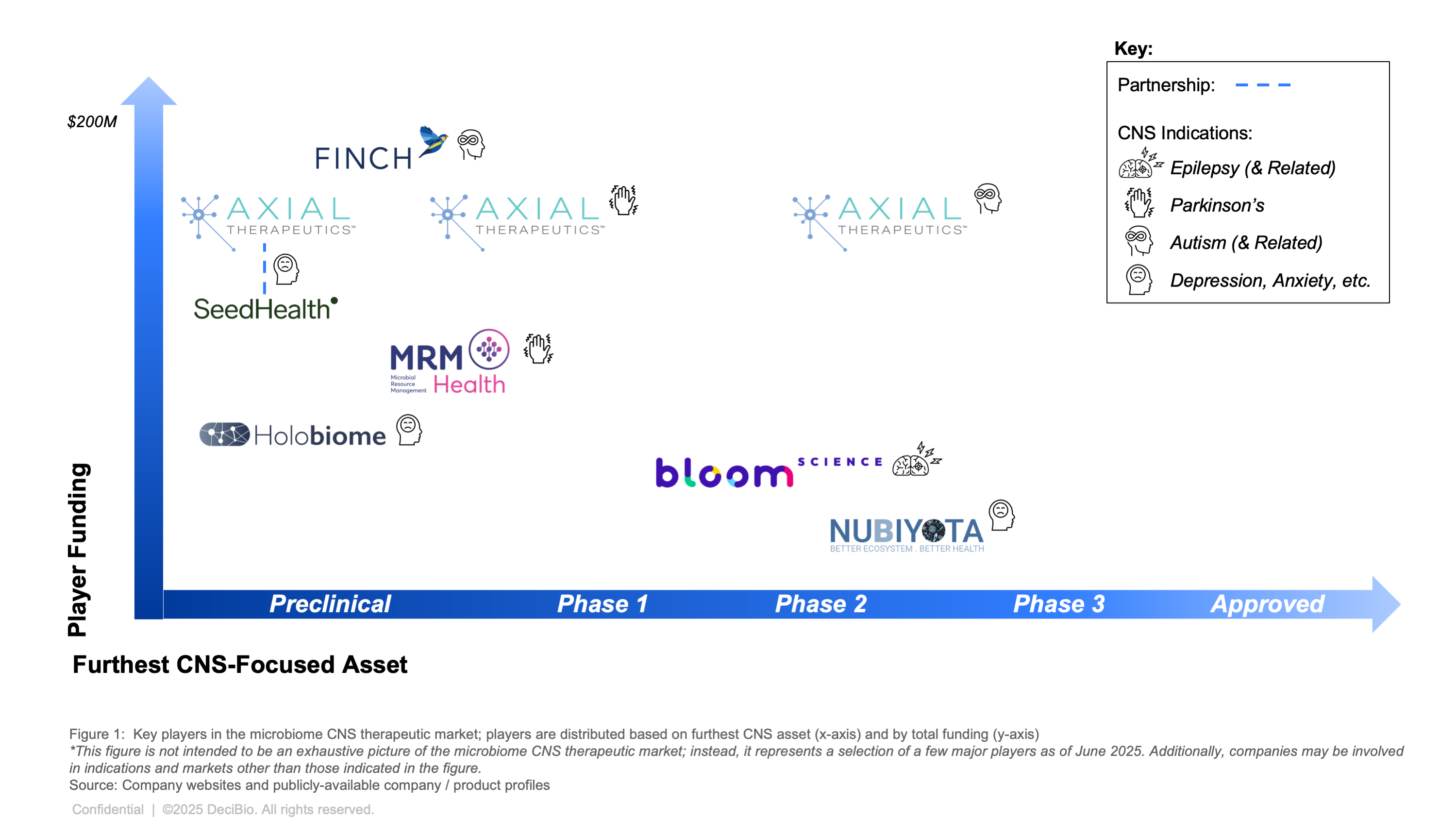
Several key players in the microbiome space are progressing neurology pipelines across CNS indications, with some assets reaching as far as Phase 2 (trials ongoing). Among them include Axial Therapeutics, whose pipeline includes a Phase 2 Autism-associated irritability asset and a preclinical Parkinson’s asset.3 Axial has partnered up with Seed Health (a probiotic company evaluated at over $1B) to jointly develop next generation microbial therapeutics to target the microbiome-gut-brain axis for mental health.4 NuBiyota's Phase 2 study is underway to evaluate changes in depression and anxiety symptoms upon administration with their Microbial Ecosystem Therapeutic (MET).5 Meanwhile, Bloom Science is advancing its epilepsy pipeline into Phase 2 trials, including a candidate for Dravet Syndrome, based on preliminary trial findings.6
Nevertheless, the microbial therapeutic landscape remains uncertain, with no approved assets for any CNS conditions to date and notable companies facing significant financial challenges — including 4D Pharma, a leader in the development of live biotherapeutics until their delisting from the Nasdaq in 2022.7 Despite these headwinds, investment and pipeline development in microbiome-focused CNS therapeutics continues. Growing evidence of the microbiome’s role in Alzheimer’s, Parkinson’s, and epilepsy is establishing a scientific foundation for therapeutic development and potential market differentiation.
Current State of Research
The nascent, yet evolving science behind the microbiome and various neurological conditions is promising. Research suggests that the microbiome may indirectly modulate the CNS environment, contributing to conditions associated with certain disorders and providing a potential pathway for treatment and / or prevention.
Alzheimer’s Disease
In 2023, it was estimated that more than 6.5 million Americans suffer from Alzheimer’s Disease (AD), with nearly ⅓ of those over the age of 85 having AD. While the genes APP, PSEN1, and PSEN2 can potentially cause AD, a combination of genetics and environmental factors are necessary to cause the disease. The brain’s microglia, or immune cells, maintain a healthy environment by patrolling for cellular debris. They can be activated by other immune cell signals, which in moderation is healthy, but in aging brains, microglia activation can be prolonged. This indicates an unnecessary response that could actually lead to brain distress and diseases like AD.
Animal studies led by Rodney W. Johnson at the University of Illinois tested how mice’s microglia responded to changes in diet to further test the gut-brain axis. Gut bacteria can convert fiber into short-chain fatty acids (SCFAs), which improve memory in animals and promote brain function.8 Similar to aging humans, aging mice express dysregulated microglia. Johnson’s team fed mice (both healthy and elderly) diets high in fiber, and results indicated improved microglia regulation for both groups, however the mechanism of the SCFA is to be solved. It is unknown if they impact the brain through direct BBB interactions, secondary communication with other bodily systems that ultimately improve brain function, or a combination of both; the method(s) of interaction additionally could vary based on the specific SCFA in question.
The metabolics associated with AD and the microbiome are an additional area of exploration. Dr. Rima Kaddura-Daouk at Duke University has found that individuals with AD have a larger build up of secondary bile-acid (BA) in their blood and less production of primary BAs in their liver, compared to healthy individuals. Bacteria in the gut-microbiome break down the liver’s produced BAs (which come from cholesterol) into these secondary BAs, which are associated with cognitive decline when sufficiently elevated. Additionally, the type of BA can have either neuro-protective or toxic properties - e.g., DCA can interfere with the brain’s gab junction and the BBB. However, the mechanisms of these pathways are yet to be fully fleshed out.9
Parkinson’s Disease
In the United States alone, a conservative estimate of 1 million individuals have Parkinson’s Disease (PD), a chronic brain disorder that impacts motor control. These symptoms relate to a loss of neurons that produce dopamine, leading to irregular brain activity. Similar to many neurological disorders, it is unknown what causes PD, likely a combination of genetic and environmental factors. Potential relevant genes include LRRK2, PARK7, PINK1, PRKN, SNCA, among others.
Zachary D. Wallen’s review of the implications of metagenomics and PD demonstrates various pathways in the gut that can ultimately play a role in a PD patient’s brain. Through conducting deep shotgun sequencing followed by metagenome-wide associate studies across nearly 500 PD and ~230 control individuals, their team evaluated how microbiota differ between the populations and support the existence of the gut-brain axis. Similarly to Johnson’s study around SCFAs for AD patients, this review highlights that the microbiome of PD patients lacks SCFA producing bacteria, observing up to a 7 fold reduction in multiple SCFA producing species. Additionally, they found that some species known to become opportunistic pathogens, such as Escherichia coli, Klebsiella pneumoniae and Klebsiella quasipneumoniae, were elevated in PD populations.10
A study conducted by Dayoon Kwon at UCLA found similar results when analyzing the gut microbiota of 85 PD individuals, further validating the importance of SCFAs to reduce systemic inflammation that can lead to the progression of PD. Findings supported that a diet with greater fiber intake increases SCFA-producing bacteria in PD populations. The anti-inflammatory properties of SCFAs could ultimately promote normal microglia development and support a healthier CNS. On the other hand, they found that high sugar diets can increase the presence of pro-inflammatory bacteria (e.g., within Klebsiella). While this information does have potential impact on earlier-diagnosed PD patients, the investigators note that the microbiome is more entrenched and less responsive as the disease progresses.11
The evidence of a connection between PD and the gut microbiome continues to be studied, with recent findings suggesting that α-synuclein proteins, a signal of PD, can manifest in clumps in the gut before the disease develops. The connection continues through other organs in the body, for cells in the appendix naturally produce high levels of this protein, and those who have had appendectomies are up to 20% less likely to develop PD.12
Epilepsy
The World Health Organization estimates that over 50 million people worldwide have epilepsy, with 80% of these patients inhabiting low and middle-income countries.13 The gut-brain axis has diagnostic and treatment implications for epilepsy, which is defined as recurrent (at least 2), unprovoked seizures, which are generated by abnormal electrical activity. While research studies tend to be small (<30 subjects) when investigating the microbiome and epilepsy, there have been substantial findings indicating that those who suffer from epilepsy can have differences in their microbiome compared to healthy subjects, especially for the 30-40% of epilepsy patients whose epilepsy is medication resistant.14
For example, Changci Zhou at the University of South Carolina, and researchers at Hunan’s Children’s Hospital, evaluated the gut microbiota of 10 children with focal epilepsy before and after treatment (oral oxcarbazepine) and found that the pre-treated group had a greater abundance of some bacteria (e.g., Actinobacteria phylum, Streptococcus) and lacked other species (e.g., Anaerostipes, Faecalibacterium). Following 3 months of treatment, there were no significant differences anymore between the control and post-treatment groups.15
In animal models, researchers such as J. Medel-Matus at UCLA, have exposed rats to chronic restraint-stress to heighten susceptibility to seizures, and found that when the fecal contents from stressed donors were transplanted into the gastrointestinal tract of pathogen-free rats, the recipients were more susceptible to seizures and had prolonged seizure donation. Conversely, intestinal microbiota transplantation from non-stressed rats to their stressed counterparts had a beneficial effect in reducing duration of seizures of the stressed rats.16
As for treatment, the KD (ketogenic diet) diet (a 2:1 or up to 4:1 fat intake compared to other macronutrients) has been an effective interventional strategy to promote seizure control that is being utilized in clinical practice today.17 The ketogenic diet is particularly effective for drug-resistant pediatric epilepsy, though its long-term metabolic effects, due to its fasting-mimicking nature, and challenges with implementation can limit its broader use. When evaluating the microbiome’s evolution during the KD diet, Gong X and other researchers at Sichuan University, found decreases in the abundance of some bacteria which were previously elevated in the epileptic cohort (e.g., Bifidobacterium, Akkermansia, Actinomyces) and an increase in the abundance of others (e.g., Subdoligranulum, Dialister).18 The optimum KD diet ratio, and the importance of implementing fiber into the KD diet, continues to be studied.
Looking Ahead: Precision Medicine’s Role
The existing literature indicates a significant connection between the microbiome and the brain, and even into other conditions such as multiple sclerosis, psychiatric disorders, and autism spectrum disorder. While some interventions have proved tentatively effective (e.g., the KD diet in epilepsy), the field has a ways to go. Due to the multifactorial nature of neurological conditions, a microbiome “solution” will likely involve the interactions between scores of microbes, maybe even millions.19 After identification, complex microbiome signatures likely affect brain function via immune-mediated signaling pathways, which are mechanisms that still demand further R&D.20 Understanding and harnessing this level of complexity will require new precision tools, such as advanced bioinformatics and mathematical modeling. Regulatory considerations, patient-specific microbiome baselining, and longitudinal sampling will also be critical in translating these insights into clinical application.
Further, taking a precision medicine approach to the microbiome may yield powerful advantages for patient stratification; understanding the role of the microbiome in individual variability in drug response (IVDR) / adverse drug reactions could offer enormous benefits in clinical management. This is especially true in the context of CNS conditions, which are highly prone to this variability, and where preliminary studies indicate that microbiota may play a key role.21
Conclusion
It is well established that the microbiome plays an important role in the CNS via the gut-brain axis, and ongoing research is beginning to suggest that these interactions may significantly contribute to several neurological disorders. While the degree to which this connection can be exploited for drug development is still unknown, several companies are making progress in the space with assets ranging from early discovery to Phase 2.
Precision medicine tools, such as NGS and advanced bioinformatics, will continue to be vital to understanding how the microbiome can impact complex, multifactorial neurological conditions. Despite uncertainties, the microbiome’s potential to influence neurological health offers hope for a new class of precision therapeutics.
1. https://pubmed.ncbi.nlm.nih.gov/34104888/
2. https://pmc.ncbi.nlm.nih.gov/articles/PMC10620799/
3. https://www.axialtx.com/our-programs/pipeline/
5. https://nubiyota.com/pipeline/
6. https://bloomscience.com/science/
8. https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2020.00025/full
9. https://www.nia.nih.gov/news/beyond-brain-gut-microbiome-and-alzheimers-disease
10. https://www.nature.com/articles/s41467-022-34667-x
11.https://pubmed.ncbi.nlm.nih.gov/38649365/
12. https://www.nature.com/articles/d41586-025-01253-2
13. https://www.who.int/news-room/fact-sheets/detail/epilepsy
14. https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1276551/full
16. https://onlinelibrary.wiley.com/doi/10.1002/epi4.12114
17. https://www.mdpi.com/2072-6643/16/9/1258?utm
18. https://pubmed.ncbi.nlm.nih.gov/33894293/
21. https://www.nature.com/articles/s41392-023-01619-w
Note: DeciBio Consulting, its employees or owners, or our guests may hold assets discussed in this article/episode. This article/blog/episode does not provide investment advice, and is intended for informational and entertainment purposes only. You should do your own research and make your own independent decisions when considering any financial transactions.







.png)


